
By Jake Poore
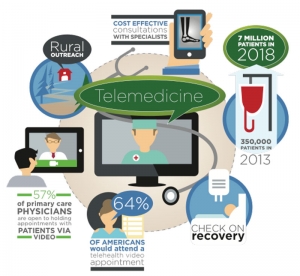
Telemedicine is one of the top trends in healthcare. The growing industry is expected to attract 7 million patients by 2018, up from 350,000 in 2013. This type of technology allows physicians to evaluate and communicate with patients remotely, using screens.
Convenience makes this option attractive to both physicians and patients alike— In fact, in a recent survey, 64% of Americans reported they would attend a telehealth video appointment, and 57% of primary care physicians said they are open to holding appointments with patients via video.
Additionally, the ability to hold appointments via video has many applications, from cost-effective consultations with specialists, to outreach in rural communities. High tech healthcare is on the rise; however, high tech is not always high touch. In other words, technology can sometimes take away from focusing on the human—from staying in touch with the person at the heart of each interaction.
An ILS focus group asked 12 patients to share their opinions on telemedicine. Everyone shared their positive experiences and their excitement about the new technology. That is, until one man spoke up from the back of the room and said, “My experience wasn’t quite like the rest.”
John, a man in his early 50s, had been healthy all his life—eating well, exercising five times a week—until one day at the gym, he collapsed on the treadmill. John was having a heart attack. He was rushed to the ER, thinking, “How could this happen to ME?”
John had quadruple bypass surgery. The procedure, though serious, was a great success. In the recovery room, John drifted in and out of consciousness as he began to wake from his surgery. Through the fog, he heard a voice saying, “…hello? Hello? John? Can you hear me, John? How are you feeling?”
John looked around the room, but couldn’t see anyone there. Who was this person? How did they know his name? Although he was meant to be recovering from a heart attack, his heart rate began to soar through the roof. Confused, John wondered if he was hallucinating from the anesthesia. “Am I losing my mind?” he thought.
“Who ARE you?” John said to the voice in the room. Without answer, the voice began giving him information about his bypass surgery, chart, vitals, etc. John looked at the TV, and saw a physician speaking. Still groggy from the medicine, John thought it was a TV character. As it turns out, the voice on the TV was John’s physician speaking to him using telemedia, updating him on important post-operation information.
John expressed to the focus group that he wished he had been warned of this ahead of time, while he was still coherent, before the surgery. Instead, he was scared, confused, and on top of that, he missed important information about his surgery due to his grogginess.
Even in the age of technology, it is important to keep in mind the human side of healthcare. Remember our Human Business Human® technique which is to always enter and exit on the human; make sure to start with a warm welcome and ensure all patient questions are answered before surgery—including explaining any new technology being used. To exit on the human, make sure they leave knowing all the important post-op information, and schedule a follow-up to check on their recovery process.
There is a right and a wrong way to leverage new and exciting technology. John’s story is one of the ways that employing new technology without thinking about the human at the center of the interaction can go very wrong. At the end of the day, healthcare workers are in the “people” business.
As telemedicine continues to catch on, offering greater convenience for both patients and healthcare professionals, we must remember that technology should always align with human needs, not replace them.





