
By Kim Court
If you ask 50 people to define “the Patient Experience”, you’ll get 50 different answers. While there are many definitions, we’ve adopted what is considered to be the most widely accepted definition, from the Beryl Institute, which reads:
The Patient Experience is the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.
If you read that definition slowly and really think about every word, it becomes clear that creating a meaningful patient experience is more than simply telling healthcare employees to just “be nicer.”
But that’s often what we do when we seek to improve the patient experience. We turn to a quick-fix script of things to say or do and then we launch a new program or initiative in the hopes of boosting patient satisfaction scores.
And it works for a short while … until it doesn’t.
Then, employees go back to doing what they’ve always done and patient satisfaction scores ebb and flow like the ocean tides.
 Moving the needle on patient experience, in a way that is meaningful and sustainable, requires a shift in thought. It can’t just be another program or initiative or checklist of what to do or say. It has to become who we are as a healing organization.
Moving the needle on patient experience, in a way that is meaningful and sustainable, requires a shift in thought. It can’t just be another program or initiative or checklist of what to do or say. It has to become who we are as a healing organization.
In order to significantly improve the patient experience, we must apply the same rigor to service excellence, kindness, and compassion as we do to clinical excellence and expertise.
After all, patients assume clinical excellence and expertise, but they also expect to be treated with kindness, respect, and dignity. In the patient’s mind, both clinical excellence and service excellence are weighted with equal importance in their patient experience journey.
The Two Strands of Patient Experience
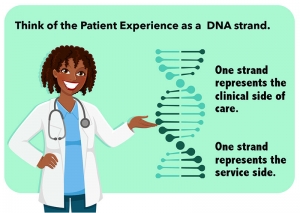
If patients don’t sense the compassion, kindness, and courtesy, then in the patient’s eyes your team’s expertise, efficiency, accuracy, and precision will fall short. And they will judge their standard of care based on this failing.
This new definition of the Patient Experience, one that encompasses the sum of all interactions across the continuum of care, demands both clinical excellence AND compassionate care be delivered in a new, elevated, human standard from the perspective of the patient.
For maximum impact over a sustained period of time, we must bridge the gap between these two strands. We do this by meeting the patient’s expectations on clinical care and expertise, while exceeding their expectations on service or kindness. It’s not enough to just focus on patients. We must create a culture, an environment, where we look at every experience from the patients’ point of view.
Everybody is focused on the bedside and the doctors and nurses, but what many organizations fail to recognize is that people are walking in and out of the front doors of hospitals and they’re scared. They are at their most vulnerable and are literally at the mercy of their care team, and that includes employees that care directly for patients and those that work behind the scenes in non-clinical areas. Patients (and families) take for granted they will be treated with clinical expertise; but they now demand that they are treated with kindness, dignity, and respect by everyone on the care team.
Flipping the Lens and Moving Toward PATIENT-DRIVEN Care
 Many in healthcare embrace the concept of being “patient-centered.” In fact, being patient-centered is a little like the Golden Rule which says: Treat others the way you would want to be treated.
Many in healthcare embrace the concept of being “patient-centered.” In fact, being patient-centered is a little like the Golden Rule which says: Treat others the way you would want to be treated.
The former assumes that what patients want is exactly what we would want. Sometimes that may be true, but often, it’s not.
While it’s not always possible to ask every patient what they prefer, there are tools and techniques that help flip the lens on the Patient Experience. One example is our Patient Experience Mapping process.
 Patient Experience Mapping is a technique where we take an intensive look at how patient’s experience care – from their vantage point. We ride on a gurney, travel in a wheelchair, lay on an MRI table, get an x-ray, walk the halls, use crutches, wait in the reception area, navigate the facility, survey patients and employees, eat the food, use the public restroom etc.
Patient Experience Mapping is a technique where we take an intensive look at how patient’s experience care – from their vantage point. We ride on a gurney, travel in a wheelchair, lay on an MRI table, get an x-ray, walk the halls, use crutches, wait in the reception area, navigate the facility, survey patients and employees, eat the food, use the public restroom etc.
We do all of these things with the intent of seeing, hearing, smelling, and experiencing things from the perspective of the patient.
When we share the Patient Experience Mapping(c) process with care teams, it gives them a firsthand glimpse into what patients see, hear, and experience at their care facility or health system. And more importantly, it opens their eyes to the parts of their facility they may not even consider as part of the patient experience.
For example, before patients ever see a doctor or a nurse, it’s quite possible they’ve seen or interacted with many other people on the care team, including: valet parking attendants, security guards, hospital volunteers, housekeepers, gift shop attendants, transporters, front desk reception, the bill payment staff, etc.
How each of these employees interacts with patients (and family members) can dramatically affect the patient experience. Are your employees set up for success to deliver what patients want? Or are they stuck in “job task” mode moving through their day performing job task after job task?
Too often, employees are focused solely on job tasks and not connected to their purpose in a healing environment.
Every member of the care team (clinical and non-clinical) has a role in shaping the patient experience.
This technique of flipping the lens offers an invaluable opportunity to move away from being simply patient-centered and, instead, move toward being more patient-driven.
This is what the volume to value shift is all about. It’s a movement from episodic care to a complete care experience. Whether you use a technique like our Patient Experience Mapping or something similar, it is imperative to bridge the gap between clinical expertise and service excellence because today’s healthcare consumers have choices.
By and large, hospitals and care facilities are all clinically excellent. Where the opportunity to differentiate lies is in an organization’s ability to deliver kindness and courtesy as astutely as they deliver medical expertise to not only meet expectations on the clinical side but exceed expectations on the service side.





